The Trending With Impact series highlights Aging (Aging-US) publications that attract higher visibility among readers around the world online, in the news, and on social media—beyond normal readership levels. Look for future science news about the latest trending publications here, and at Aging-US.com.
—
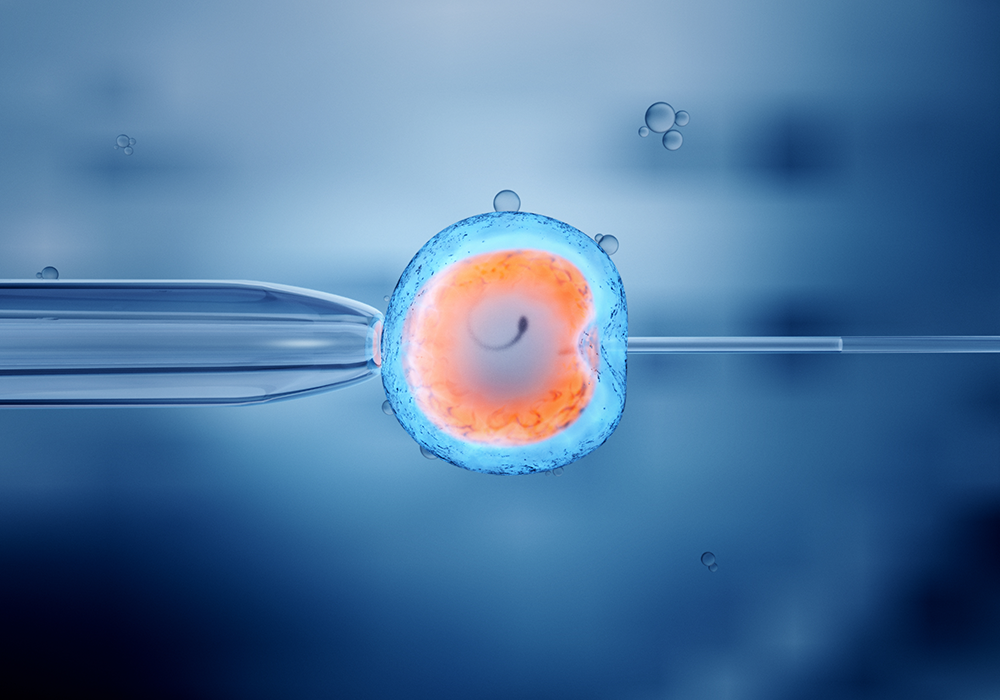
In a day and age when women and men are beginning families later in the life cycle, women of advanced age (or with some health conditions) often have trouble becoming pregnant. Today, in vitro fertilization (IVF) is a widely-used form of assisted reproductive technology. This manual process of fertilization is achieved first by combining an egg and a sperm outside of the uterus and then helping the fertilized egg become implanted in the uterus.
The world’s first IVF baby was born in Lancashire, England, in 1978. Since then, this technique has solved reproductive issues for millions of women and men around the world. While this procedure has helped build many families, there is a subset of reproductively challenged women who exhibit resistance to IVF. Researchers have observed accelerated ovarian aging in women who demonstrate a poor ovarian response (POR) to IVF.
“These women are labeled ‘poor ovarian response’ (POR) or ‘poor responders’ due to a combination of low parameters of ovarian reserve and previous low oocyte yield after ovarian stimulation.”
In previous small-scale cohort and in vitro studies, exposure to platelet-rich plasma (PRP) has demonstrated improvements in ovarian tissue repair, regeneration and follicular development. In a new study, published in Aging (Aging-US) on March 22, 2022, researchers—from Acibadem Maslak Hospital, Acibadem University, IVI RMA New Jersey, Thomas Jefferson University, and Yale School of Medicine—sought to validate these small-scale results by assessing the effects of intra-ovarian injection of autologous PRP in a cohort of 510 women with POR. Their trending research paper can be found in Volume 14, Issue 6, entitled, “Ovarian reserve parameters and IVF outcomes in 510 women with poor ovarian response (POR) treated with intraovarian injection of autologous platelet rich plasma (PRP).”
The Study
This prospective observational study took place in Acibadem Maslak Hospital in Istanbul, Turkey, in 2020. The study’s inclusion criteria admitted women who were diagnosed with POR, between 30 and 45 years old, had at least a one-year history of infertility, and had at least one ovary. After the exclusion criteria were accounted for, 510 women with POR were included in the study. Patients were divided into three groups for subgroup assessment: patients younger than 38 years old, patients between 38 and 42 years old and patients between 42 and 45 years old.
Before IVF, autologous PRP was administered to participants through intra-ovarian injections. (Learn more about PRP and IVF materials and methods in the study.) The team then assessed the effects of PRP on ovarian reserve parameters and IVF outcomes. Ovarian reserve parameters included antral follicle count (AFC), ovarian volume, serum anti-Müllerian hormone (AMH) level, and serum follicle-stimulating hormone (FSH) level. IVF outcomes were defined by the number of oocytes retrieved (an oocyte is an immature ovum, or egg cell) and the number and quality of embryos that developed, including embryos in cleavage and blastocyst stages.
The Results
Compared to baseline measures before treatment, PRP injections resulted in higher AFC, higher serum AMH, lower serum FSH, and a higher number of mature oocytes and cleavage/blastocyst stage embryos. In this cohort of women with POR, the PRP intervention yielded a total pregnancy rate of 20.5% and a sustained implantation/livebirth rate of 12.9%.
“After PRP injection, 22 women (4.3%) conceived spontaneously, 14 (2.7%) were lost to follow up, and 474 (92.9%) attempted IVF. Among women who attempted IVF, 312 (65.8%) generated embryos and underwent embryo transfer, 83 (17.5%) achieved a pregnancy, and 54 (11.4%) achieved sustained implantation/live birth (SI/LB).”
The researchers found that the greatest increase in IVF outcomes was seen in women 38 years old or younger. They also performed a receiver operating characteristic curve analysis and found that the cut-off for patients who would not benefit from PRP was 40 years old. The authors explained that this was due to a lack of ovarian response.
Conclusion
The researchers suggest that PRP may be considered for IVF cycles in women with POR, especially for those younger than 38 years old. However, the authors also caution that PRP should not be recommended as part of routine treatments until further prospective randomized trials test for clinical efficacy in wider clinical applications. Intra-ovarian injection of autologous PRP may someday be the standard of care for women with POR seeking IVF.
“In conclusion, intraovarian injection of autologous PRP might be considered in women with POR. The ideal population that may benefit from this approach can be summarized as patients <40 years old, with an FSH < 21.2 mIU/mL, AMH > 0.23 ng/ml, with at least one antral follicle, and a mean ovarian volume > 4.30 cm3.”
Click here to read the full research paper published by Aging (Aging-US).
AGING (AGING-US) VIDEOS: YouTube | LabTube | Aging-US.com
—
Aging (Aging-US) is an open-access journal that publishes research papers bi-monthly in all fields of aging research. These papers are available at no cost to readers on Aging-us.com. Open-access journals have the power to benefit humanity from the inside out by rapidly disseminating information that may be freely shared with researchers, colleagues, family, and friends around the world.
For media inquiries, please contact [email protected].